Platelet-Activating Factor
 The term 'platelet-activating factor' was first
introduced in 1972 to define a then unknown metabolite, which induced the aggregation of blood platelets released from
basophils stimulated with immunoglobulin E.
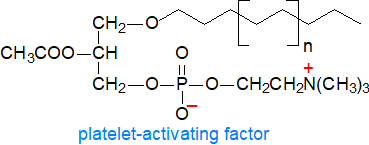
In 1979, independently in the laboratories of D.J. Hanahan, J. Benveniste and F. Snyder,
a phospholipid identified as 1‑O‑alkyl-2-acetyl-sn-glycero-3-phosphocholine, an ether analogue of
phosphatidylcholine, was shown to be responsible for this activity
and for that of a compound that had been termed ‘antihypertensive polar renal lipid’.
It was thus one of the first complex lipids known to act via a receptor and have signalling properties and not simply to be a structural
component of membranes or to act via its hydrolysis products.
The term 'platelet-activating factor' was first
introduced in 1972 to define a then unknown metabolite, which induced the aggregation of blood platelets released from
basophils stimulated with immunoglobulin E.
In 1979, independently in the laboratories of D.J. Hanahan, J. Benveniste and F. Snyder,
a phospholipid identified as 1‑O‑alkyl-2-acetyl-sn-glycero-3-phosphocholine, an ether analogue of
phosphatidylcholine, was shown to be responsible for this activity
and for that of a compound that had been termed ‘antihypertensive polar renal lipid’.
It was thus one of the first complex lipids known to act via a receptor and have signalling properties and not simply to be a structural
component of membranes or to act via its hydrolysis products.
In the light of what is now known of the manifold properties of this lipid in animal tissues, platelet-activating factor or PAF is not an appropriate name, as it is present in many cell types, including those for host defence such as macrophages and mast cells, but it has stuck. It is vital for some key physiological processes, but in contrast, it is a potent pro-inflammatory mediator that is implicated in innumerable disease states involving inflammation, allergic responses, cell damage or death, and shock.
PAF is an unusual lipid in many ways, although it can be considered to be a special case of the more abundant ether lipids with shared biosynthetic pathways. In general, the alkyl groups tend to be mainly saturated and C16 or C18 in chain-length, although trace vinyl ether (plasmalogen) forms have been detected. There are few other examples of acetic acid esterified directly to glycerol amongst natural lipids in animal tissues (see here..), and short-chain fatty acids other than acetate (e.g., propionyl, butyryl) are only occasionally found in position sn-2 of PAF. However, oxidatively truncated phospholipids, i.e., with a short-chain, ω-aldehydo-fatty acid in position sn‑2 and formed by spontaneous scission of long-chain hydroperoxides, can behave in a PAF-like manner. PAF is present at very low levels in unstimulated animal tissues, and it can be hard to detect experimentally, but it has not been identified definitively in plants.
1. Biosynthesis of Platelet-Activating Factor
PAF is synthesised by a variety of cells, but mainly those for defence, such as platelets, endothelial cells, neutrophils, monocytes and macrophages, from alkylacyl-phospholipids synthesised in the endoplasmic reticulum after introduction of the alkyl group in peroxisomes as with other ether lipids.
In the main two-step (so-called 'remodelling') pathway, which is always triggered in both acute and chronic inflammation, membrane-bound acetyl-CoA:lyso-PAF acetyltransferases (e.g., LPLAT9 or LPCAT2) on the nuclear membrane or the endoplasmic reticulum in contact with the cytoplasm catalyse the transfer of an acetyl residue from acetyl-CoA to 1-O-alkyl-sn-glycerol-3-phosphocholine (lyso-PAF). This intermediate is generated by the action of a dual-purpose phospholipase A2 on 1-O-alkyl-2-acyl-phosphatidylcholine, with a high specificity for those molecular species with arachidonic acid in position sn-2. There is thus a link between the metabolism of PAF and subsequent eicosanoid production.
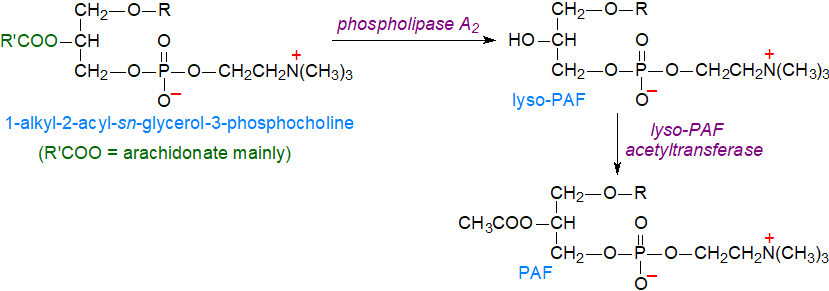 |
| Figure 1. Biosynthesis of platelet-activating factor by the remodelling pathway. |
The acetyltransferase also acts as CoA-independent transacylase to relocate the cleaved arachidonate to position sn-2 of either lysophosphatidylcholine or lysophosphatidylethanolamine, although the lysoplasmalogen form of phosphatidylethanolamine may be the main acceptor before the vinyl bond is reduced and the head group is exchanged. In addition, lyso-PAF can be generated from 1-O-alkyl-2-acyl-phosphatidylcholine by the action of CoA-independent or CoA-dependent transacylases (reversal of an acyl-CoA acyltransferase reaction), a sequence of reactions that can be compared to the Lands' cycle. It is not known how PAF is then translocated from the interior of the cell to the exterior, where it is encounters its receptor on endothelial cells and leukocytes for signalling purposes; monocytes release most of their PAF.
The main source of PAF is the isoform LPLAT9 of the acetyltransferase, which is inducible and is considered to be pro-inflammatory, as it catalyses a very rapid synthesis of PAF in macrophages following phosphorylation of the enzyme by protein kinase Cα upon stimulation by endogenous G-protein-coupled receptor ligands or by lipopolysaccharides during bacterial infection. Only when the cells are subjected to acute inflammatory stimulation does the enzyme produce PAF in appreciable amounts as a possible critical step at the onset or in the early stages of inflammatory responses. PAF is produced continuously at low levels by the isoform LPLAT8, which is constitutively expressed in the lungs, where it produces PAF (and dipalmitoyl-phosphatidylcholine) essential for respiration under non-inflammatory conditions.
There is an alternative biosynthetic mechanism for PAF production (‘de novo’ pathway) that contributes the physiological levels of PAF needed for normal cellular operation and starts with acetylation of 1-O-alkyl-sn-glycero-3-phosphate, i.e., an intermediate in the biosynthesis of ether lipids and a lysophosphatidic acid analogue, to form 1‑O‑alkyl-2-acetyl-sn-glycero-3-phosphate by means of a different acetyltransferase from that using lyso-PAF as substrate, i.e., an acetyl-CoA:alkyl-lysoglycerophosphate acetyltransferase. As with other ether lipids, the product is dephosphorylated by an alkylacetylglycerophosphate phosphohydrolase with formation of 1‑O‑alkyl-2-acetyl-sn-glycerol, which can be converted to PAF by a mechanism analogous to that for the biosynthesis of phosphatidylcholine but utilizing a CDP-choline alkylacetylglycerol cholinephosphotransferase different from that using diacylglycerols as substrate. This pathway occurs mainly in the brain and kidney and is important during continuous triggering of inflammatory cascades as in the development of inflammation-related disorders. It does not generate free arachidonic acid for eicosanoid synthesis.
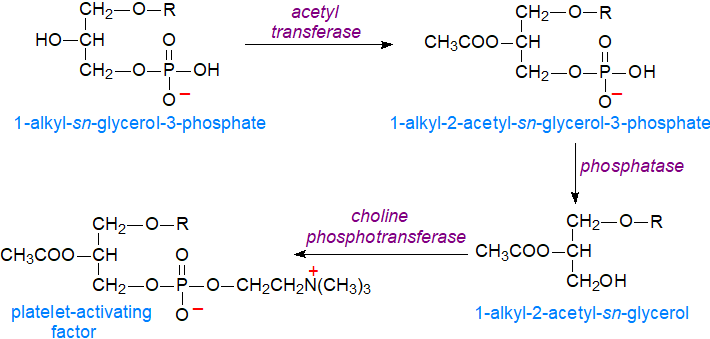 |
| Figure 2. Biosynthesis of platelet-activating factor by the de novo pathway |
Production of PAF is limited by acetyl hydrolases (see below), and with the involvement of so many synthetic and catabolic mechanisms, regulation of PAF levels is a highly complicated process.
2. Biochemical Functions of Platelet-Activating Factor
Receptor: PAF at the surface of the plasma membrane was one of the first intact phospholipids known to have messenger functions, i.e., in which the signalling results from the molecule binding to a receptor, rather than from physico-chemical effects on the plasma membrane or other membranes of the cell. There is a strict structural requirement for binding to its unique trans-membrane G‑protein coupled receptor (PAFR), which is expressed by numerous cells, including all those of the innate immune system, to promote downstream signalling on target cells. Thus, there is a specificity of nearly three orders of magnitude for the ether bond in position sn-1 of PAF in comparison to the 1-acyl analogue, together with considerable specificity for a short acyl chain in position sn-2 and for the phosphocholine head group. In endothelial cells, the receptor is found in both cell surface and large endosomal membranes and is coupled to intracellular Gαq and Gαi heterotrimeric G-proteins, which send distinct yet synergistic signals into target cells such as leukocytes and platelets. On the other hand, some of its activities appear to be independent of the receptor, and in primitive marine animals such as corals, which do not possess platelets, PAF and lyso-PAF are produced in response to external stresses.
The PAF response is controlled to some extent by variable expression of the PAF receptor on cell surfaces, as the relevant gene generates two distinct transcripts, PAFR transcript 1 and PAFR transcript 2, because of the presence of two different promoters. In human tissues, peripheral leukocytes and differentiated eosinophilic cell lines express PAFR transcript-1 primarily, while heart, lungs, spleen, and kidney tissue express PAFR transcript-2 mainly.
Inflammation: Much of the research into signalling by PAF has been concerned with acute and chronic inflammation, which occurs in most animal tissues, and can be considered as both beneficial and pathophysiological as it is necessary for the day-to-day protection from pathogenic insults. PAF is presumed to have evolved as part of a defensive mechanism in the innate host immune system, but when produced in an uncontrolled manner, it can be harmful, and it has been implicated in the pathogenesis of several disease states, ranging from allergic reactions to stroke, sepsis, myocardial infarction, cancer, colitis, HIV infection, and the effects of ultra-violet radiation. It can mediate metabolic events in a juxtacrine, paracrine autocrine, or endocrine manner. Eicosanoids produced as a by-product of PAF biosynthesis are also mediators of inflammation and may act synergistically with PAF.
Initially, PAF was found to cause aggregation of platelets at concentrations as low as 10-11M following its release from immunoglobulin E‑stimulated basophils, and it induced a hypertensive response at similarly low levels. Indeed, it is almost always active by 10-9M as an intercellular messenger, and more generally, it is now recognized that its primary role is to mediate intercellular interactions. For example, when PAF binds to its own receptor (PAFR), the Gq protein component of this combines with phospholipase Cβ to hydrolyse phosphatidylinositol 4,5-bisphosphate to inositol trisphosphate and diacylglycerol that causes an increase in intracellular Ca2+ downstream of the cell and activation of protein kinase C. In addition, the rise in Ca2+ induces phospholipase A2 (cPLA2α) to release arachidonic acid for synthesis of eicosanoids and lysophosphatides, which can serve as substrates for further PAF synthesis. Signalling through PAFR inhibits the conversion of ATP to cAMP by adenylate cyclase and prevents the activation of protein kinase A and its associated signalling events. PAF is now known to influence many different types of metabolic events in this manner, including glycogen degradation, reproduction, brain and retinal function, and blood circulation. Although its inflammatory reactions have received most study, PAF operates in the central system in relation to neuronal development and to long-term potentiation, a process that is essential for memory formation.
 Much
recent work has been concerned with PAF as a mediator of inflammation and in the mechanism of the immune response;
it can stimulate human inflammatory cells at concentrations as low as 10-14M.
Binding to its receptor on inflammatory cells induces very rapid (within 30 seconds) production of further PAF via enhanced
LPLAT9 mediated by phosphorylation by protein kinase C, and in turn, the increased PAF levels induce subsequent inflammatory cascades.
The amount of PAF produced by cellular stimuli of various kinds is dependent on the nature of the cell and agonist.
Although it was once thought to be a hormone that acted locally, as it was found initially only on the surface of activated cells so restricting
the inflammatory response, it is now known to be transported in extracellular vesicles to other tissues to exert its effects.
As PAF can activate inflammasomes directly, i.e., independently of its receptor PAFR, to release the pro-inflammatory cytokines
IL-1β and IL-18, this may explain why some PAFR antagonists do not block PAF-mediated inflammation in clinical trials.
Much
recent work has been concerned with PAF as a mediator of inflammation and in the mechanism of the immune response;
it can stimulate human inflammatory cells at concentrations as low as 10-14M.
Binding to its receptor on inflammatory cells induces very rapid (within 30 seconds) production of further PAF via enhanced
LPLAT9 mediated by phosphorylation by protein kinase C, and in turn, the increased PAF levels induce subsequent inflammatory cascades.
The amount of PAF produced by cellular stimuli of various kinds is dependent on the nature of the cell and agonist.
Although it was once thought to be a hormone that acted locally, as it was found initially only on the surface of activated cells so restricting
the inflammatory response, it is now known to be transported in extracellular vesicles to other tissues to exert its effects.
As PAF can activate inflammasomes directly, i.e., independently of its receptor PAFR, to release the pro-inflammatory cytokines
IL-1β and IL-18, this may explain why some PAFR antagonists do not block PAF-mediated inflammation in clinical trials.
It has a key role in the destabilizing and rupture of atherosclerotic plaques that leads to acute cardiovascular events, and an increase in the concentration of PAF has been observed in the blood of patients with acute myocardial infarction and arrhythmia. In relation to asthma, PAF can act directly as a chemotactic factor and indirectly by stimulating the release of other inflammatory agents. Administration of PAF can produce many of the symptoms observed in asthma, including bronchoconstriction, mucus hypersecretion and inflammation of bronchi, probably via the formation of leukotrienes as secondary mediators. In pregnancy, PAF contributes to the maturation of the oocyte, but excessive elevation in amniotic fluid mediates inflammation that can lead to preterm delivery in both humans and mice.
PAF can be an anti-obesity factor, which acts through stimulation of its receptor in brown but not white adipose tissue, and reduction in this activity may be responsible for increasing adiposity with age. Another view is that PAF has a contradictory role in regulating body weight and thence obesity that depend upon concentration. At the normal controlled levels of PAF in adipose tissue, there is a beneficial autocrine effect that leads to the maintenance of healthy adipose tissue, but under conditions of oxidative stress and inflammation, high levels of PAF produced by blood cells and the endothelium cause inflammation and thrombosis through paracrine action and juxtracrine signalling.
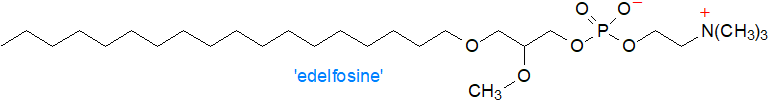
As a pro-inflammatory mediator, PAF has been implicated in the development of cancer, especially that of the skin, where it takes part in transmitting the immunosuppressive signal of UV irradiation from the skin surface to the immune system in keratinocytes and thence in inducing mast cell migration in vivo. Elevated levels of the PAF receptor are present in tumour cells and cells that infiltrate tumours with negative impacts upon the efficacies of chemotherapy and radiation therapy, resulting in promotion of tumour cell proliferation, production of survival signals, differentiation of immunosuppressive neutrophils, migration of vascular cells and formation of new vessels. In experimental models, it has been shown that blocking of the PAF receptor reduces tumour growth and increases animal survival. A synthetic analogue of PAF, 1‑O‑octadecyl-2-O-methyl-rac-glycero-3-phosphocholine (‘edelfosine’) is a potent anticancer agent in animal models by causing selective apoptosis of cancer cells while sparing healthy cells, but it appears to be too toxic for use with humans. On the other hand, this may be merely the first step in the development of new ether-linked drugs, and analogues in which the phosphocholine moiety is replaced by a carbohydrate are showing promise for their therapeutic potential. Nutraceuticals containing natural PAF agonists are under development.
By increasing the permeability of the blood-brain barrier, PAF facilitates inflammation in the brain. By binding to its receptor, it enhances calcium entry into cells and drives neuronal development, but dysregulation is a factor in ocular disorders, including age-related macular degeneration and diabetic retinopathy, and when in deficit, and it can influence neurodegeneration as in multiple sclerosis, dementia, Alzheimer’s disease, and Parkinson’s disease. Chronic inflammation induced by PAF causes progressive neuronal loss, cognitive decline and/or motor dysfunction, so it is hoped that targeting the PAF signalling pathway through use of agonist for its receptor will have preventative and therapeutic benefits.
Other activities: PAF is reported to be an important regulator of membrane channels and transporters (collectively named the transportome). The nature of the alkyl group in position sn-1 may be important to such processes, and it has been established that C16- and C18-PAF cause death to cerebellar granule neurons, although they signal through different pathways. In addition, PAF receptor signalling can be either pro- or anti-apoptotic, depending upon the nature of the sn-1 alkyl moiety, probably because of differential binding of each homologue to the receptor. In relation to the physiology of reproduction, it modulates ovulation, fertilisation, preimplantation, implantation and parturition in females, while it is present in spermatozoa and may be required for sperm motility in males.
Phosphatidylethanolamine analogues of PAF have been studied, but they are much less potent. A further comparable signalling molecule, N‑acetylsphingosine, is produced by a CoA-independent transacetylase, which transfers the acetyl group of PAF to sphingosine (see our web page on ceramides). Although lyso-PAF can cause neurotoxicity and an inflammatory response, it may have opposing effects to PAF in relation to neutrophil superoxide production and platelet aggregation. Alkylacetylglycerols, analogues of 1,2-diacyl-sn-glycerols and PAF precursors, have biological activities, some of which are independent of subsequent conversion to PAF. They have been shown to promote differentiation of cultured leukaemia cells and to affect many other cell types in vitro at least, although this may in part be due to formation of metabolites. Further, they can be phosphorylated to generate 1-O-hexadecyl-2-acetyl-sn-glycero-3-phosphate, a phosphatidic acid analogue, which is thought to compete with diacylglycerols to regulate protein kinase C signalling and/or its membrane location.
1-O-Acyl analogues of PAF, i.e., with a saturated fatty acid rather than an alkyl moiety in position sn-1, are produced in tissues in amounts that surpass that of PAF, and while they may have mild proinflammatory properties, their main function appears to be to attenuate and possibly regulate PAF signalling by acting as sacrificial substrates for PAF acetylhydrolases and perhaps as endogenous PAF-receptor antagonist/partial agonists. For example, administration of alkyl-PAF causes sudden death in Swiss albino mice, but this is suppressed by administering boluses of acyl-PAF at the same time. When assayed directly, depending on the bioassay system used, the difference in potency of the acyl analogue ranged from a 100-fold to a 2000-fold decrease relative to PAF per se.
3. Catabolism of Platelet-Activating Factor
Control of PAF concentration and activity is regulated partly by tight control of its synthesis and partly by the action of PAF acetylhydrolases, three of which exist with one in plasma and two intracellular and cytosolic (all Ca2+-independent); they are classified as part of the large phospholipase A2 family of enzymes. Their main function is to remove the acetyl group from PAF to render it inert, but importantly, they do not target conventional phospholipids. One of the intracellular forms (PAF-AH(I)) is enriched in brain and is completely specific for PAF but is required for spermatogenesis and is increasingly recognized as an oncogenic factor.
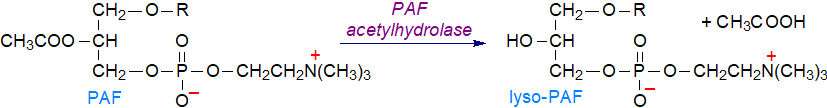 |
| Figure 3. Catabolism of platelet-activating factor. |
The second intracellular isoform (PAF-AH(II)) is expressed in virtually all tissues, but most abundantly in the liver, kidney, intestine and testis, and it has a broader specificity in that, like the plasma form, it will hydrolyse truncated acyl moieties from oxidized phospholipids (see next section). In mast cells and many other cell types, this enzyme releases enzymatically oxidized fatty acids, including eicosanoids such as F2‑isoprostane residues and hydroperoxy- or epoxy-octadecadienoyl/eicosatrienoyl moieties (lipid mediators), that are esterified to phospholipids (oxidized phospholipids), so it may have a role in allergic diseases.
The third most abundant and best characterized PAF-acetylhydrolase is the plasma form, which is associated with both circulating LDL and HDL particles and acts at the lipid-aqueous interface, where it is sometimes termed the ‘lipoprotein-associated phospholipase A2’ (Lp‑PLA2 - group VII family). This is secreted constitutively by blood cellular components and to a lesser extent by liver cells, aorta cells and adipocytes, and it a 45 KDa protein, which circulates in plasma in its active form. All three enzymes hydrolyse unmodified fatty acyl residues up to 5 or 6 carbon atoms long in the sn-2 position also, albeit relatively slowly, although even this restriction is relaxed when the terminal-end of the fatty acyl moiety is oxidized (i.e., aldehydic or carboxylic), such as in the oxidatively truncated phospholipids. By removing the latter within cells, PAF acetylhydrolase protects cells from apoptosis. PAF-acetylhydrolases can act also as trans-acetylases to transfer short-chain fatty acids from PAF to ether/ester-linked lysophospholipids. One further enzyme, alkaline sphingomyelinase, renders PAF inert but by removing the phosphocholine moiety.
It has been suggested that the other products of PAF hydrolases, lysophosphatidylcholines, may be pro-atherogenic, and in support of the latter view, large-scale epidemiological studies have found that elevated plasma PAF-acetylhydrolase/Lp-PLA2 levels are associated with an increased risk of coronary disease, stroke and mortality. In contrast, one effect of the plasma form may be to remove oxidized phospholipids from lipoproteins and atherosclerotic plaques that might otherwise contribute to their inflammatory properties, and while oxysterols accumulate as atherosclerotic lesions mature, formation and destruction of oxidized phosphatidylcholines is a continuous process in both early and advanced lesions. The balance between pro- and anti-inflammation is obviously critical. There are also conflicting reports of this enzyme and cancer, as it can act as either a tumour promoter or a tumour suppressor depending on the context. Some but not all species of lyso-PAF accumulate in various tissues in Niemann-Pick disease type C1, possibly as secondary storage metabolites.
Expression of these enzymes is upregulated at the transcriptional level by mediators of inflammation in response to inflammatory stimuli, but they are susceptible to oxidative inactivation. Decreased levels are associated with various diseases, including asthma, systemic Lupus erythematosus and Crohn’s disease. In clinical and preclinical studies, inhibition of Lp-PLA2 has shown promise in diabetic macular oedema and Alzheimer’s disease.
The ether linkage in the lysophospholipid can be cleaved oxidatively by the microsomal alkylglycerol monooxygenase to yield a fatty aldehyde, which is then further oxidized to the corresponding acid as described in our web page on ether lipids.
4. Oxidatively Truncated Phospholipids
PAF-like molecules with some biological properties are produced in tissues by non-enzymatic oxidation of polyunsaturated fatty acids in phospholipids and in phosphatidylcholine especially, resulting in cleavage near the first double bond to leave a short-chain acid with a terminal aldehyde (or carboxyl) group in position 2, a so‑called ‘core aldehyde’, together with a volatile aldehyde. This process is discussed in greater detail in our web page dealing with oxidized phospholipids. While the biosynthesis of PAF is tightly regulated, the various non-enzymatic oxidation reactions that produce core aldehydes are essentially uncontrolled. Such compounds are formed in plasma lipoproteins and human atherosclerotic lesions, and indeed, they were first identified as the components of oxidized LDL that mediate many of the pro-inflammatory and pro-atherogenic effects reported for these lipoproteins.
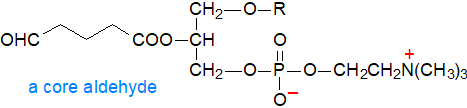
Oxidatively truncated phospholipids have been reported to possess a wide range of actions, many of which correspond to those of PAF. They bring about platelet aggregation at nanomolar concentrations by binding to the PAF receptor, and they may be involved in thrombosis and acute coronary events by inducing proliferation of smooth muscle cells. By means of a mechanism that is independent of the PAF receptor, they are pro-apoptotic and have a substantial influence on regulated cell death, while as might be expected, they have a disruptive effect upon cell membranes. In contrast, they can prevent endotoxin shock induced by exposure to bacterial lipopolysaccharides in vivo.
Catabolism: The oxidized fatty acids in position sn-2 are removed by the PAF-acetylhydrolases described above to yield short-chain aldehydo fatty acids (unesterified) and lysophosphatidylcholine, and in plasma, the lecithin-cholesterol acyltransferase (LCAT) acts in a similar way, presumably as a detoxification mechanism for oxidized lipoproteins. Thirdly, the lysosomal phospholipase A2 can remove the fatty acids from position sn-1 of these lipids.
4. Analysis
The main problem in the analysis of PAF is the very low concentration at which it is present and biologically active in tissues (as low as 10-11M), but separation by reversed phase liquid chromatography and detection by mass spectrometry with selected reaction monitoring in negative ion mode or related technologies may be an answer, although there remains a need for high through-put methodology. Comparable approaches have been used for oxidatively truncated phospholipids.
Suggested Reading
- Adamantidi, T., Grabrucker, A.M. and Tsoupras, T. Targeting platelet activating factor signaling for therapeutic benefits in neurodegenerative disorders. Front. Biosci. (Landmark Ed), 30, 38300 (2025); DOI.
- Davies, S.S. and Guo, L.L. Lipid peroxidation generates biologically active phospholipids including oxidatively N-modified phospholipids. Chem. Phys. Lipids, 181, 1-33 (2014); DOI.
- Deng, M. and others. Platelet-activating factor (PAF) mediates NLRP3-NEK7 inflammasome induction independently of PAFR. J. Exp. Med., 216, 2838-2853 (2019); DOI.
- Harishkumar, R., Hans, S., Stanton, J.E., Grabrucker, A.M., Lordan, R. and Zabetakis, I. Targeting the platelet-activating factor receptor (PAF-R): antithrombotic and anti-atherosclerotic nutrients. Nutrients, 14, 4414 (2022); DOI.
- Kimura, T., Jennings, W. and Epand, R.M. Roles of specific lipid species in the cell and their molecular mechanism. Prog. Lipid Res., 62, 75-92 (2016); DOI.
- Kono, N. and Arai, H. Platelet-activating factor acetylhydrolases: An overview and update. Biochim. Biophys. Acta, Lipids, 1864, 922-931 (2019); DOI.
- Lordan, R., Tsoupras, A., Zabetakis, I. and Demopoulos, C.A. Forty years since the structural elucidation of platelet-activating factor (PAF): historical, current, and future research perspectives. Molecules, 24, 4414 (2019); DOI.
- Marathe, G.K., Chaithra, V.H., Ke, L.-Y. and Chen, C.-H. Effect of acyl and alkyl analogs of platelet-activating factor on inflammatory signaling. Prostaglandins Other Lipid Mediators, 151, 106478 (2020); DOI.
- Ramakrishnan, A.V.K.P., Varghese, T.P., Vanapalli, S., Nair, N.K. and Mingate, M.D. Platelet activating factor: A potential biomarker in acute coronary syndrome? Card. Ther., 35, 64-70 (2017); DOI.
- Rangholia, N., Leisner, T.M. and Holly, S.P. Bioactive ether lipids: primordial modulators of cellular signaling. Metabolites, 11, 41 (2021); DOI.
- Suzuki, T., Taketomi, Y., Yanagida, K., Yoshida-Hashidate, T., Nagase, T., Murakami, M., Shimizu, T. and Shindou, H. Re-evaluation of the canonical PAF pathway in cutaneous anaphylaxis. Biochim. Biophys. Acta, Lipids, 1870, 159563 (2025); DOI.
- Travers, J.B., Rohan, J.G. and Sahu, R.P. New insights into the pathologic roles of the platelet-activating factor system. Front. Endocrinol., 11, 624132 (2021); DOI.
- Tsoupras, A. and others. Re-assessing the role of platelet activating factor and its inflammatory signaling and inhibitors in cancer and anti-cancer strategies. Front. Biosci. (Landmark Ed), 29, 345 (2024); DOI.
- Upton, J.E.M., Grunebaum, E., Sussman, G. and Vadas, P. Platelet activating factor (PAF): a mediator of inflammation. Biofactors, 48, 1189-1202 (2022); DOI.
- Yang, X.R., Tu, Y.B., Liang, N., Li, L.L., Zhang, J., Xu, J.Y. and Li, C.M. Lp-PLA2 in the cancer landscape: From molecular mechanisms to therapeutic potential (Review). Int. J. Oncol., 67, 87 (2025); DOI.
 |
© Author: William W. Christie |  |
|
| Contact/credits/disclaimer | Updated: October 2025 | ||
© The LipidWeb is open access and fair use is encouraged but not text and data mining, AI training, and similar technologies.
